Eye Movement Desensitization and Reprocessing (EMDR)
Eye Movement Desensitization and Reprocessing (EMDR)1) is an evidence-based psychotherapy treatment modality used to effectively treat a wide range of psychological issues, including post-traumatic stress disorder (PTSD). Its efficacy has been extensively studied and documented.
This therapy works by activating different networks in the brain that store and process traumatic material while simultaneously using a process of Bilateral stimulation (BLT)2) using: eye movements, tones, and/or tactile taps to stimulate the processing of memories related to the trauma.
In EMDR therapy, the therapist helps the client to identify connected thoughts, memories, images, and sensations related to the traumatic experience, then guides them through a series of alternating bilateral stimulation exercises.
Additionally, EMDR can also be used in combination with other treatments such as cognitive behavioral therapy for individuals on waiting lists for more intensive mental health services.
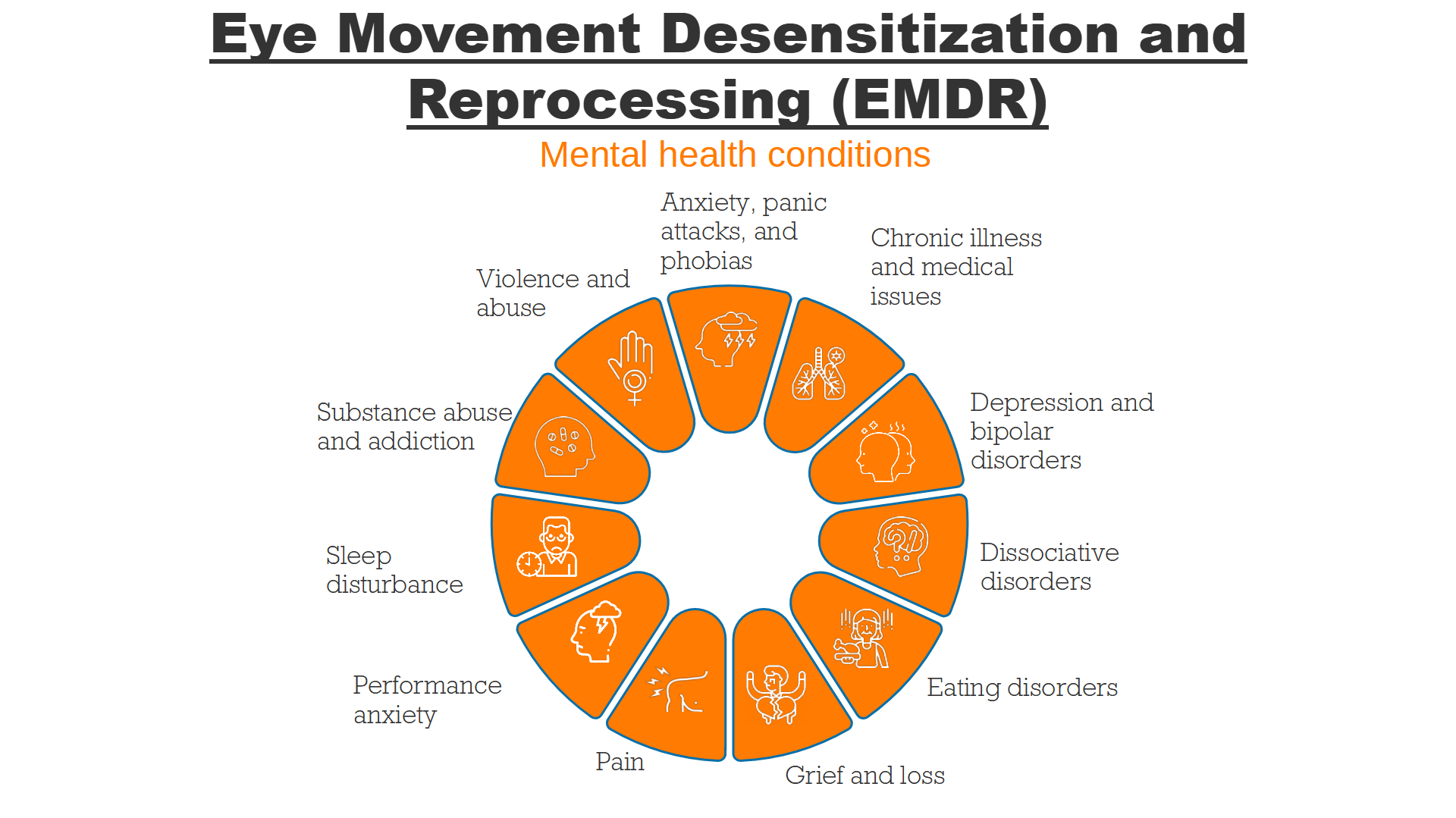
EMDR has established its effectiveness in treating trauma and PTSD in children and adults, alongside other mental health conditions such as:
- Anxiety, panic attacks, and phobias
- Chronic illness and medical issues
- Depression and bipolar disorders
- Dissociative disorders
- Eating disorders
- Grief and loss
- Pain
- Performance anxiety
- Sleep disturbance
- Substance abuse and addiction
- Violence and abuse
Although some may prefer traditional treatments like medications and talk therapy, others may find that EMDR can accelerate the process of healing. EMDR therapy is considered a safe form of treatment and aims to leave you with the emotions, understanding, and perspectives that promote healthy, positive change.
What does the process look like?
Research has established a strong link between the proper application of the Eye Movement Desensitization and Reprocessing (EMDR) standard protocol and positive therapeutic outcomes. Consequently, strict adherence to this protocol is essential for maintaining EMDR’s empirical effectiveness and robustness (Maxfield, et al., 2002). The protocol consists of eight structured phases, each incorporating specific procedures and standardized questions. These phases are outlined in Table 1.
The Eight Phases of the EMDR Standard Protocol
| Phase | Description |
|---|---|
| Phase 1: Patient History and Treatment Planning | Gathering patient history, identifying symptoms, formulating a case conceptualization, and creating a treatment plan. |
| Phase 2: Preparation | Establishing a therapeutic alliance, providing psychoeducation on trauma and EMDR therapy, and enhancing emotional regulation skills. |
| Phase 3: Assessment | Identifying target memories, activating traumatic memory components (image, negative cognition, positive cognition, emotions, bodily sensations), and assessing distress levels using a 0-10 scale. |
| Phase 4: Desensitization | Processing traumatic memories through dual-attention tasks (e.g., guided bilateral eye movements) until distress is no longer reported. |
| Phase 5: Installation | Reinforcing a positive cognition associated with the traumatic memory. |
| Phase 6: Body Scan | Conducting a full-body scan to identify and release residual distress linked to the memory. |
| Phase 7: Closure | Ensuring patient stability post-session and making necessary follow-up arrangements. |
| Phase 8: Reevaluation | Reviewing progress and assessing treatment effectiveness in subsequent sessions. |
Overview of the EMDR Process
The primary goal of EMDR therapy is to minimize distress associated with traumatic memories while strengthening positive self-referential beliefs. The therapist facilitates the process by guiding the patient through structured memory activation and bilateral stimulation exercises.
The process begins with Phase 1, where the therapist gathers the patient’s history, identifies PTSD symptoms, and selects target memories for treatment. In Phase 2, the patient is prepared for trauma processing through psychoeducation and coping strategies.
Phase 3 involves assessing the identified traumatic memory. The therapist asks the patient to recall the most distressing aspects of the memory while evaluating their negative and positive cognitions, emotions, and bodily sensations. The level of distress is measured using the Subjective Units of Disturbance Scale (SUDS) ranging from 0 (no distress) to 10 (extreme distress).
In Phase 4, desensitization begins. The patient processes the memory using bilateral stimulation (typically rapid eye movements guided by the therapist’s hand or a light bar). After each set of eye movements, the therapist assesses spontaneous patient responses and encourages further processing until the distress associated with the memory is neutralized (SUDS score of 0).
Phase 5 focuses on reinforcing a positive cognition using the Validity of Cognition (VoC) scale, which ranges from 1 (completely untrue) to 7 (completely true). The patient recalls the traumatic memory while mentally repeating the positive cognition alongside bilateral stimulation until the VoC score is maximized.
Phase 6 involves a body scan to identify any lingering distress. If any physical discomfort is detected, additional processing is applied. In Phase 7, the session is concluded, ensuring that the patient is stable and comfortable before ending.
The final phase, Phase 8, occurs at the start of the next session. The therapist reviews the previous session’s outcomes, evaluates progress, and determines the need for further treatment.
Treatment Duration and Effectiveness
EMDR therapy sessions typically last between 60 and 90 minutes and may be conducted individually or in group settings. While randomized controlled trials on group EMDR are limited, emerging evidence suggests that it effectively reduces PTSD symptoms (Kaptan, et al., 2021) . Sessions are traditionally scheduled weekly, though intensive formats with daily or twice-daily sessions have also been shown to be effective (Bongaerts, et al., 2017).
Studies indicate that some individuals no longer meet PTSD diagnostic criteria after just five EMDR sessions following a single-incident traumatic event (Nijdam, et al., 2012). However, for individuals with PTSD stemming from multiple traumatic experiences, treatment typically requires 8 to 12 sessions in routine clinical practice. For a comprehensive description of the EMDR protocol, refer to Shapiro (2018).
EMDR example sessions:
Dr. Stephen Dansiger - EMDR Therapy: Phase 1 through 7 (Completed Target)
EMDR Therapy: Demonstration & Step-by-Step Walkthrough
EMDR Therapy Demonstration: Phases 1-8
EMDR Therapy Demonstration: Phases 3-7
EMDR Therapy Demonstration: Full Protocol to Address Present Prong Complaint
EMDR Therapy Phases 3-7 Demonstration (Coping with Political Stressors Presenting Issue)
Francine Shapiro
Francine Shapiro, Ph.D.3), is a clinical psychologist, research scientist and innovator who is the credited with the development of Eye Movement Desensitization and Reprocessing (EMDR) therapy (debated/controversial “Revisiting the Origins of EMDR”4)).
As the founder of the EMDR label, Dr. Shapiro has conducted research demonstrating its efficacy for treating conditions such as post-traumatic stress disorder (PTSD), anxiety disorders, specific phobias and other psychological traumas. She has also developed an approach to understanding how memories become distorted over time and how they can be reframed ever more effective ways with EMDR therapy.
In addition to her research into EMDR, Dr. Shapiro is the author of several books on mental health topics related to trauma resolution, including Getting Past Your Past: Take Control of Your Life with Self-Help Techniques from EMDR Therapy (2012)(Shapiro, F., 2012). Through her work in promoting EMDR therapy around the world, Dr. Shapiro has had a profound impact on helping individuals address even long-standing traumas quickly, effectively and without much need for medications or psychotherapy substitutes.
Bessel van der Kolk
EMDR gained medical mainstream acceptance with the neuroimaging studies of PTSD and of Dissociative Identity Disorder by Bessel van der Kolk. He received the first grants from the National Institutes of Health to do large studies about EMDR and Yoga.5)6)
An important implication of these findings is that successful treatment of PTSD does not reduce arousal at the limbic level, but instead, enhances the ability to differentiate real from imagined threat. Bessel van der Kolk7)
Reddit Forums
With such a large client and userbase it is well worth going through the EMDR reddit forum to explore what the clients who are doing the therapy are experiencing or what the ones who are looking into getting it are afraid about. https://www.reddit.com/r/EMDR/
Critique of EMDR and Francine Shapiro
A summary, historical overview and and the current states of affair on the topic :
A hard look at EMDR and its unscrupulous founder via Neuro Transmissions
A more elaborate and historical view on the claims from F. Shapiro is available via “Revisiting the Origins of EMDR”8)
References
Adams, R., Ohlsen, S., & Wood, E. (2020). Eye Movement Desensitization and Reprocessing (EMDR) for the treatment of psychosis: A systematic review. European Journal of Psychotraumatology, 11(1). https://doi.org/10.1080/20008198.2019.1711349
America, G. M. (2021). Prince Harry opens up about EMDR therapy in new show l GMA [Video]. In YouTube. https://youtu.be/QGiqBazdPGw?si=575Ve2qBDLVEb7BR
Arkowitz, H., & Lilienfeld, S. O. (2012, August 1). EMDR: Taking a closer look. Scientific American. https://www.scientificamerican.com/article/emdr-taking-a-closer-look/
Bernhard, M. (2023). The enigmatic method. VQR Online. https://www.vqronline.org/reporting-articles/2023/06/enigmatic-method
Blum, D., & Park, S. (2022, September 19). What is E.M.D.R.? Understanding the Trauma Therapy Practice. The New York Times. https://www.nytimes.com/2022/09/19/well/emdr-therapy.html
Carey, B. (2019, July 11). Francine Shapiro, developer of eye-movement therapy, dies at 71. The New York Times. https://www.nytimes.com/2019/07/11/science/francine-shapiro-dead.html
Chen, L., Zhang, G., Hu, M., & Liang, X. (2015). Eye movement desensitization and reprocessing versus cognitive-behavioral therapy for adult posttraumatic stress disorder. Journal of Nervous & Mental Disease, 203(6), 443–451. https://doi.org/10.1097/nmd.0000000000000306
Chen, Y.-R., Hung, K.-W., Tsai, J.-C., Chu, H., Chung, M.-H., Chen, S.-R., Liao, Y.-M., Ou, K.-L., Chang, Y.-C., & Chou, K.-R. (2014). Efficacy of eye-movement desensitization and reprocessing for patients with posttraumatic-stress disorder: A meta-analysis of randomized controlled trials. PLoS ONE, 9(8), e103676. https://doi.org/10.1371/journal.pone.0103676
Contributors to Wikimedia projects. (2023, December 21). Purple hat therapy. Wikipedia. https://en.wikipedia.org/wiki/Purple_hat_therapy
Cuijpers, P., Veen, S. C. van, Sijbrandij, M., Yoder, W., & Cristea, I. A. (2020). Eye movement desensitization and reprocessing for mental health problems: A systematic review and meta-analysis. Cognitive Behaviour Therapy, 49(3), 165–180. https://doi.org/10.1080/16506073.2019.1703801
Dansiger, Dr. S. (2018). Dr. Stephen Dansiger - EMDR therapy: Phase 1 through 7 (completed target) [Video]. In YouTube. https://youtu.be/B122emzNPSU?si=YI2IG4RvBtIKM2H7
Denniston, J. (2019). Is EMDR more effective than wait list control and treatment as usual with posttraumatic stress disorder symptoms? (Thesis, Concordia University, St. Paul).
Devilly, G. J., Ono, M., & Lohr, J. M. (2014). The use of meta-analytic software to derive hypotheses for EMDR. Journal of Behavior Therapy and Experimental Psychiatry, 45(1), 223–225. https://doi.org/10.1016/j.jbtep.2013.10.004
EMDR, V. (2014). EMDR interview Francine Shapiro [Video]. In YouTube. https://youtu.be/8GUd5hhnkVE?si=JTI3WNNuxzvEmd7l
Enevoldsen, R. (2014). Francine Shapiro EMDR for trauma eye movement desensitization and reprocessing [Video]. In YouTube. https://youtu.be/bWf39Pqcoqg?si=8iP8K99ge4de9tA3
Eye movement desensitization and reprocessing (EMDR) therapy. (2017, May 25). //Https:%%//%%Www.Apa.Org//. https://www.apa.org/ptsd-guideline/treatments/eye-movement-reprocessing
Faretta, E., & Dal Farra, M. (2019). Efficacy of EMDR therapy for anxiety disorders. Journal of EMDR Practice and Research, 13(4), 325–332. https://doi.org/10.1891/1933-3196.13.4.325
Foreman, J. (1998, September 14). New therapy for trauma is doubted. Judy Foreman. https://judyforeman.com/columns/new-therapy-trauma-doubted/
Freund, B. (2017). Francine shapiro interview on EMDR [Video]. In YouTube. https://youtu.be/IigQZKLXIck?si=LSMg720XKUOOh_yF
Gunter, R. W., & Bodner, G. E. (2009). EMDR works . . . But how? Recent progress in the search for treatment mechanisms. Journal of EMDR Practice and Research, 3(3), 161–168. https://doi.org/10.1891/1933-3196.3.3.161
Herbert, J. (2000). Science and pseudoscience in the development of eye movement desensitization and reprocessing Implications for clinical psychology. Clinical Psychology Review, 20(8), 945–971. https://doi.org/10.1016/s0272-7358(99)00017-3
Kenchel, J. M., Domagalski, K., Butler, B. J., & Loftus, E. F. (2020). The messy landscape of eye movements and false memories. Memory, 30(6), 678–685. https://doi.org/10.1080/09658211.2020.1862234
Landin-Romero, R., Moreno-Alcazar, A., Pagani, M., & Amann, B. L. (2018). How does eye movement desensitization and reprocessing therapy work? A systematic review on suggested mechanisms of action. Frontiers in Psychology, 9. https://doi.org/10.3389/fpsyg.2018.01395
Lee, C. (n.d.). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. https://doi.org/10.1016/j.cpr.2015.10.003
Lee, C. W., & Cuijpers, P. (2013). A meta-analysis of the contribution of eye movements in processing emotional memories. Journal of Behavior Therapy and Experimental Psychiatry, 44(2), 231–239. https://doi.org/10.1016/j.jbtep.2012.11.001
Lewey, J. H., Smith, C. L., Burcham, B., Saunders, N. L., Elfallal, D., & O’Toole, S. K. (2018). Comparing the effectiveness of EMDR and TF-CBT for children and adolescents: A meta-analysis. Journal of Child & Adolescent Trauma, 11(4), 457–472. https://doi.org/10.1007/s40653-018-0212-1
Logsdon, E., Cornelius-White, J. H. D., & Kanamori, Y. (2023). The effectiveness of EMDR with individuals experiencing substance use disorder: A meta-analysis. Journal of EMDR Practice and Research, 17(1), 21–32. https://doi.org/10.1891/emdr-2022-0046
Luber, M., & Shapiro, F. (2009). Interview with Francine Shapiro: Historical overview, present issues, and future directions of EMDR. Journal of EMDR Practice and Research, 3(4), 217–231. https://doi.org/10.1891/1933-3196.3.4.217
M. Rosen, G. (2023). Revisiting the origins of EMDR. Journal of Contemporary Psychotherapy, 53(4), 289–296. https://doi.org/10.1007/s10879-023-09582-x
McLEAN, D. (1985, February 13). Aiming at superachievers : NLP: Influencing anybody to do just about anything. Los Angeles Times. https://www.latimes.com/archives/la-xpm-1985-02-13-vw-4747-story.html
Menon, S. B., & Jayan, C. (2010). Eye movement desensitization and reprocessing: A conceptual framework. Indian Journal of Psychological Medicine, 32(2), 136–140. https://doi.org/10.4103/0253-7176.78512
Mikelson, B. (2018, April 13). IMPLEMENTING EMDR THERAPY: REFLECTIONS AFTER TRAINING WITH FRANCINE SHAPIRO - Blog. EMDR & Beyond. https://emdrandbeyond.com/blog/2018/4/13/reflections-on-training-with-francine-shapiro
RodaleBooks. (2011). Getting Past Your Past / Francine Shapiro [Video]. In YouTube. https://youtu.be/nylajeG6uFY?si=0LYFRKMbTFLqYpxQ
Opheim, E., Andersen, P. N., Jakobsen, M., Aasen, B., & Kvaal, K. (2019). Poor quality in systematic reviews on PTSD and EMDR – an examination of search methodology and reporting. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.01558
Psychology training - Schema therapy. (2017, April 27). Psychology Training. https://psychology-training.com.au/
Rasines-Laudes, P., & Serrano-Pintado, I. (2023). Efficacy of EMDR in Post-Traumatic Stress Disorder: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Psicothema, 35(4), 385–396.
Rodenburg, R., Benjamin, A., de Roos, C., Meijer, A. M., & Stams, G. J. (2009). Efficacy of EMDR in children: A meta-analysis. Clinical Psychology Review, 29(7), 599–606. https://doi.org/10.1016/j.cpr.2009.06.008
Rousseau, P.-F., Boukezzi, S., Garcia, R., Chaminade, T., & Khalfa, S. (2020). Cracking the EMDR code: Recruitment of sensory, memory and emotional networks during bilateral alternating auditory stimulation. Australian & New Zealand Journal of Psychiatry, 54(8), 818–831. https://doi.org/10.1177/0004867420913623
Rubin, A. (2003). Unanswered questions about the empirical support for EMDR in the treatment of PTSD: A review of research. Traumatology, 9(1), 4–30. https://doi.org/10.1177/153476560300900102
Scelles, C., & Bulnes, L. C. (2021). EMDR as treatment option for conditions other than PTSD: A systematic review. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.644369
Seidler, G. H., & Wagner, F. E. (2006). Comparing the efficacy of EMDR and trauma-focused cognitive-behavioral therapy in the treatment of PTSD: A meta-analytic study. Psychological Medicine, 36(11), 1515–1522. https://doi.org/10.1017/s0033291706007963
Sepehry, A. A., Lam, K., Sheppard, M., Guirguis-Younger, M., & Maglio, A.-S. (2021). EMDR for depression: A meta-analysis and systematic review. Journal of EMDR Practice and Research, 15(1), 2–17. https://doi.org/10.1891/emdr-d-20-00038
Shapiro, F. (1989). Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. Journal of Traumatic Stress, 2(2), 199–223. https://doi.org/10.1002/jts.2490020207
Shapiro, F. (2014). The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: Addressing the psychological and physical symptoms stemming from adverse life experiences. The Permanente Journal, 18(1), 71–77. https://doi.org/10.7812/tpp/13-098
Shapiro, F. (2015, May 5). Vita. EMDR Institute - EYE MOVEMENT DESENSITIZATION AND REPROCESSING THERAPY. https://www.emdr.com/vita/
Sikes, C., & Sikes, V. (2003). EMDR: Why the controversy? Traumatology, 9(3), 169–182. https://doi.org/10.1177/153476560300900304
Skeptic. (2014, May 21). Eye Movement Magic. Skeptic. https://www.skeptic.com/eskeptic/14-05-21/#feature
Verstrael, S., van der Wurff, P., & Vermetten, E. (2013). Eye movement desensitization and reprocessing (EMDR) as treatment for combat-related PTSD: A meta-analysis. Military Behavioral Health, 1(2), 68–73. https://doi.org/10.1080/21635781.2013.827088
Wadji, D. L., Martin-Soelch, C., & Camos, V. (2022). Can working memory account for EMDR efficacy in PTSD? BMC Psychology, 10(1). https://doi.org/10.1186/s40359-022-00951-0
Warren, P. (2019, July 15). Francine Shapiro obituary. The Guardian. https://www.theguardian.com/science/2019/jul/15/francine-shapiro-obituary
Wartik, N. (1994, August 7). The amazingly simple, inexplicable therapy that just might work : Is EMDR psychology’s magic wand or just some hocus pocus? Los Angeles Times. https://www.latimes.com/archives/la-xpm-1994-08-07-tm-24471-story.html
Weber, M., Schumacher, S., Hannig, W., Barth, J., Lotzin, A., Schäfer, I., Ehring, T., & Kleim, B. (2021). Long-term outcomes of psychological treatment for posttraumatic stress disorder: A systematic review and meta-analysis - Corrigendum. Psychological Medicine, 51(16), 2946–2946. https://doi.org/10.1017/s0033291721003214
Wetherford, R. (2014). Francine shapiro EMDR interview. Psychotherapy.Net. https://www.psychotherapy.net/interview/francine-shapiro-emdr