IEMT Practitioners are encouraged to investigate and learn the different nursing models1) 2)3)(C. Riehl, 1980) in order to better understand how to systematize their work with their clients.
Nursing models have been tried and tested, updated, and adjusted by countless healthcare professionals over many decades and as such have taken on an archetypal quality. Many of the learnings and practicalities within the model's implementation can be readily applied to other healthcare disciplines of practice.
Additional Nursing Models
- Newman's Health Promotion Model
- Benner's Novice to Expert Model
- Neuman's Systems Model
- Levine's Conservation Model
- Roger's Science of Unitary Human Beings
- Johnson's Behavioral System Model
- Parse's Human Becoming Theory
- Orlando's Patient-centered Nursing Theory
Newman's Health Promotion Model (NHPM)
Newman's Health Promotion Model (NHPM)4)5)6) is a nursing theory that was developed by Margaret A. Newman7) in the late 1970s and early 1980s. The model focuses on promoting health and preventing illness by addressing the individual's unique needs and characteristics.
The NHPM is based on the idea that health is not just the absence of disease, but rather a positive state of well-being. It posits that individuals have an innate drive towards health and that nurses can facilitate this process by identifying and addressing the unique health needs of each person.
“Health is the expansion of consciousness.”Newman, 1983
The model names several key components:
- The individual: The model focuses on the individual as the primary target of health promotion efforts. It recognizes that individuals have unique characteristics, experiences, and perspectives that influence their health behaviors.
- Personal factors: The model identifies personal factors such as knowledge, attitudes, and beliefs that influence health behaviors. These factors are seen as important determinants of health and are targeted in health promotion efforts.
- Social support and relationships: The model recognizes the importance of social support and relationships in promoting health. It suggests that positive social interactions and support can positively influence health behaviors and outcomes.
- The environment: The model focuses on the role of the environment in promoting health. It recognizes that access to health services and resources, as well as the physical, social, and cultural environment, can influence health behaviors and outcomes.
- Health behaviors: The model recognizes that health behaviors, such as exercise, diet, and self-care, are important determinants of health and should be targeted in health promotion efforts.
- Health outcomes: The model focuses on the ultimate goal of health promotion, which is to improve health outcomes. It suggests that by addressing the multiple determinants of health, individuals can achieve optimal health outcomes.
The individual is seen as a unique being with unique health needs and characteristics. The environment includes the physical, social, and cultural factors that affect the individual's health. Health is defined as a positive state of well-being, and nursing is seen as a process of facilitating the individual's innate drive toward health.
In practice, the NHPM can be used to guide the development of nursing interventions and health promotion programs. The model emphasizes the importance of understanding the individual's unique needs, characteristics, and values in order to create a personalized plan of care.
The NHPM consists of three levels: the individual level, the interpersonal level, and the community level. At the individual level, the model focuses on personal factors such as knowledge, attitudes, and beliefs that influence health behaviors. At the interpersonal level, the model considers the impact of social support and relationships on health. At the community level, the model focuses on the role of the environment in promoting health, such as access to health services and resources. Overall, the NHPM emphasizes the importance of addressing the multiple determinants of health to achieve optimal health outcomes. The NHPM has been widely used and applied in a variety of settings, including hospitals, primary care, community health, and long-term care. It is considered a holistic, person-centered model that promotes health and well-being.
Benner's Novice to Expert Model
Benner's Novice to Expert Model8) (Patricia Benner, 1984)9) , also known as the Novice to Expert theory, is a nursing theory developed by Patricia Benner in the early 1980s. The theory describes the process of how nurses develop and acquire knowledge and skills throughout their careers, from novice to expert.
The model is based on the idea that nursing practice is a dynamic process and that nurses' knowledge and skills develop over time through various stages of experience.
Benner identifies five stages of nursing practice:
- Novice: At this stage, the nurse is new to the field and relies heavily on rules and step-by-step procedures to guide their practice. They lack experience and understanding of the context in which they are working.
- Advanced Beginner: The nurse has gained some experience and is starting to recognize patterns in their work, but they still rely on rules and procedures to guide their practice.
- Competent: The nurse has a deeper understanding of the context in which they are working and can begin to anticipate problems and plan accordingly. They still rely on rules and procedures, but they are able to adapt them to the specific situation.
- Proficient: The nurse has a high level of skill and experience and can act in a variety of situations. They can recognize patterns and anticipate problems, but they also rely on intuition and past experience.
- Expert: The nurse has a deep understanding of the context in which they are working and can respond quickly and effectively to new situations. They can anticipate problems and plan accordingly, and they rely on intuition and past experience.
The Novice to Expert theory emphasizes the importance of continuing education and professional development to help nurses progress through the stages of practice. It also underlines the importance of mentorship and guidance in the development of nurses as experts. The Novice to Expert model has been widely used in nursing education, practice, and research, and it is considered a valuable tool for evaluating nurses' clinical competence, and designing educational programs for nursing students and practicing nurses.
Neuman's Systems Model
Neuman's Systems Model10) 11)12) is a nursing theory developed by Betty Neuman in the 1970s (Neuman, Betty M, 2010, 5th Edition)13). The model focuses on the individual as a whole person and emphasizes the importance of understanding the person in the context of their environment.
Optimal wellness is the greater possible degree of system stability at a given point in timeNeuman, 2002
The model is based on the concept that the individual is a system made up of various subsystems, such as physical, psychological, social, and spiritual components. The model posits that the individual's health and well-being are influenced by the interactions between these subsystems and the external environment.
The model includes three main components: the individual, the environment, and the nursing process. The individual is seen as a unique being with unique needs and characteristics. The environment includes the physical, social, and cultural factors that affect the individual's health.
Betty Neuman's Systems Model includes the concept of “lines of resistance,” which refer to the various levels of protection that individuals have against stressors. These lines of resistance include physical, psychological, and social barriers that help to protect the individual from stressors and maintain system equilibrium.
- Physical line of resistance: This line of resistance includes the body's natural defense mechanisms, such as the immune system, which help to protect the individual from physical stressors such as infection.
- Psychological line of resistance: This line of resistance includes the individual's coping mechanisms, such as problem-solving skills and emotional regulation, which help to protect the individual from psychological stressors such as anxiety and depression.
- Social line of resistance: This line of resistance includes the individual's social support systems, such as family, friends, and community, which help to protect the individual from social stressors such as isolation and discrimination.
According to Neuman's theory, when stressors are encountered, and the lines of resistance are breached, the individual's system equilibrium is disrupted. The model suggests that nurses must assess the individual's lines of resistance and take appropriate action to minimize the impact of stressors and restore system equilibrium.
Optimal client system stability means the highest possible health condition achievable at a given point in timeNeuman, 2002
The model defines prevention as the identification and management of stressors that have the potential to disrupt the individual's system equilibrium, and suggests that nurses must be able to identify these stressors and take appropriate action to minimize their impact.
Neuman's Systems Model proposes three levels of prevention: primary, secondary, and tertiary prevention.
- Primary prevention: This level of prevention focuses on preventing the occurrence of stressors and the development of illness in the first place. This can be achieved by providing health education, promoting healthy lifestyles, and providing access to preventive health services.
- Secondary prevention: This level of prevention focuses on early detection and intervention to minimize the impact of stressors and illness. This can be achieved by providing screening and diagnostic services, and early treatment.
- Tertiary prevention: This level of prevention focuses on rehabilitation and recovery from illness, and preventing recurrence. This can be achieved by providing rehabilitation services, and helping patients to manage chronic conditions.
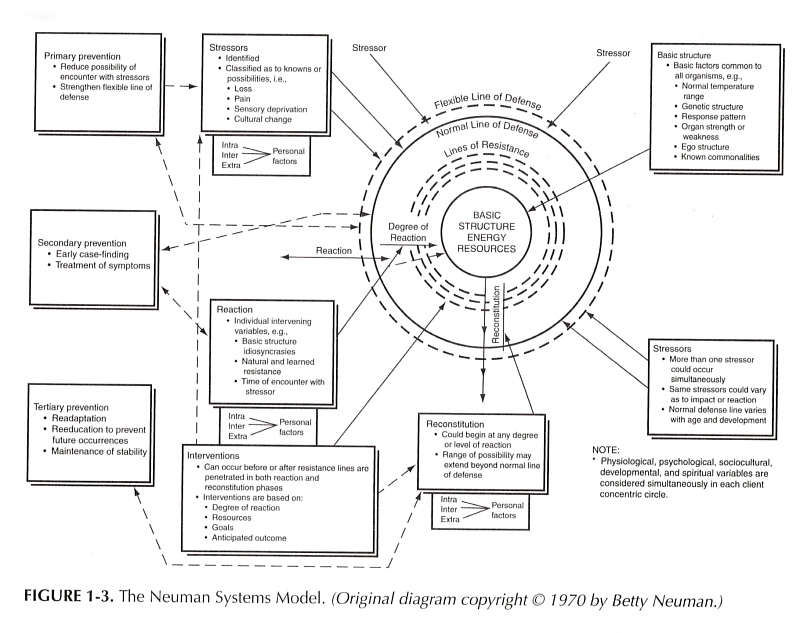
Overall, Neuman's Systems Model emphasizes the importance of prevention in maintaining health and well-being, and suggests that nurses must be able to identify and manage stressors to minimize their impact. The model also highlights the importance of providing education, promoting healthy lifestyles and providing access to preventive health services to prevent illness from occurring in the first place, provide early detection and intervention to minimize the impact of stressors and illness, and provide rehabilitation and recovery from illness and preventing recurrence.
Neuman's Systems Model is widely used in nursing practice, education, and research, and is considered a holistic, person-centered model that promotes health and well-being. It is also considered a useful tool for understanding the complex interactions between the individual, environment, and nursing care.
Levine's Conservation Model
Levine's Conservation Model14)15)16) is a nursing theory developed by Faye Glenn Levine(1920-1996) in the 1980s. The model emphasizes the importance of conservation, which refers to energy, structural integrity, personal integrity and social integrity.
The model is based on the idea that the individual is a holistic being, made up of physical, psychological, social, and spiritual components. The model posits that health and well-being are maintained through the conservation of these components.
The model includes four main components: the individual, the environment, health, and nursing. The individual is seen as a holistic being with unique needs and characteristics. The environment includes the physical, social, and cultural factors that affect the individual's health. Health is defined as a state of balance and harmony among the various components of the individual.
The nursing process includes assessment, planning, implementation, and evaluation. The model emphasizes the importance of understanding the individual's unique needs and characteristics and creating a personalized plan of care to promote health and well-being.
The prepositions of Levine's Conservation Model include:
- Holism: The model emphasizes the importance of considering the whole person, including their physical, emotional, social, and spiritual needs, when providing care.
- Homeostasis: The model posits that individuals have a natural tendency to maintain a balance or equilibrium in their lives, and that this balance can be disrupted by illness or injury.
- Adaptation: The better patients can adapt to the changes in health, the better they are able to respond to treatment and care. Every individual has unique range of adaptive responses which vary based on heredity, age, gender or challenges of an illness experience..
- Interdependence: The model recognizes that individuals are interconnected and that their actions and interactions with others can affect their ability to maintain balance.
- Culture and spirituality: The model emphasizes the importance of considering the individual's cultural and spiritual background, as well as their personal values and beliefs, when providing care.
- Preservation and promotion: The model proposes that the nurse's role is to preserve the individual's balance and promote their well-being by identifying and addressing factors that are contributing to the disruption.
According to Levine's conservation model, the individual and their environment become aligned over time through specific adaptive responses. This process, known as conservation, can occur at various levels. In the field of nursing, the goal is to assist individuals in maintaining their overall well-being with minimal effort.
The core of Levine ‘s theory is her four principles of conservation17):
- Conservation of Energy: This principle states that the individual should conserve their energy by reducing unnecessary physical and mental exertion. This includes minimizing activities that are not essential to maintaining health and well-being and maximizing rest and relaxation.
- Conservation of Structural Integrity: This principle states that the individual should maintain their physical and emotional health by preserving their structural integrity. This includes taking care of the body through proper nutrition, exercise, and hygiene, as well as protecting it from injury and illness.
- Conservation of Personal Integrity: This principle states that the individual should maintain their sense of self and personal identity by preserving their personal integrity. This includes maintaining a sense of control over one's life, making choices and decisions, and setting goals.
- Conservation of Social Integrity: This principle states that the individual should maintain their social connections and relationships by preserving their social integrity. This includes maintaining positive relationships with family, friends, and community and participating in social activities.
Overall, these principles are interrelated and aim to help individuals maintain their overall well-being by preserving their physical, emotional, and social health. By following these principles, individuals can make the most of their resources, reduce stress and improve their overall quality of life.
Levine's Conservation Model is widely used in nursing practice, education, and research, and is considered a holistic, person-centered model that promotes health and well-being. It is also considered a useful tool for understanding the complex interactions between the individual, environment, and nursing care. The theory is widely generalizable, It can be used in any setting with any human being who is suffering and willing to seek assistance from a nurse.
Roger's Science of Unitary Human Beings
Roger's Science of Unitary Human Beings18)19) is a nursing theory developed by Martha E. Rogers20) in the 1970s. The model emphasizes the holistic and unique nature of each individual, and suggests that health and illness are not fixed states, but rather are constantly changing processes.
The model is based on the idea that the individual is a open, self-organizing, and holistic system that is in constant interaction with the environment. The model views health as a dynamic state of balance and harmony between the in. It posits that the individual is a unique being with unique needs and characteristics and that health and well-being are maintained through the balance and harmony of the various components of the individual.
The model includes four main components: the individual, the environment, health, and nursing. The individual is seen as a unitary being with unique needs and characteristics. The environment includes the physical, social, and cultural factors that affect the individual's health. Health is defined as a state of balance and harmony among the various components of the individual.
The nursing process consists of six steps:
- Assessment : This step involves gathering data about the person's health status, including their physical, psychological, and social well-being. The nurse uses non-directive communication techniques, such as active listening and open-ended questions, to understand the person's subjective experience of their health and illness.
- Diagnosis : Based on the data gathered in the assessment step, the nurse identifies patterns and themes that indicate health and illness. The nurse also considers the person's unique perspective and experiences in making their diagnosis.
- Outcome Identification : The nurse works with the person to identify their desired outcomes, taking into account the person's unique perspective and experiences. Outcomes may include physical, psychological, and social well-being.
- Planning : The nurse develops a plan of care that is tailored to the person's unique needs and goals. The plan of care should be flexible and open to change as the person's needs and goals evolve over time.
- Implementation: The nurse carries out the plan of care, working in partnership with the person to promote their health and well-being.
- Evaluation: The nurse evaluates the effectiveness of the plan of care in achieving the patient's desired outcomes. The nurse also considers the patient's unique perspective and experiences in making this evaluation.
The model emphasizes the importance of understanding the individual's unique needs and characteristics and creating a personalized plan of care to promote health and well-being.
The Science of Unitary Human Beings is based on the concept of “unitary field experience” which refers to the individual's personal experience of the environment and the self. The model emphasizes the importance of the nurse-patient relationship and the nurse's role in facilitating the individual's innate drive toward health and well-being.
Rogers' Science of Unitary Human Beings is widely used in nursing practice, education, and research, and is considered a holistic, person-centered model that promotes health and well-being. It is also considered a useful tool for understanding the complex interactions between the individual, environment, and nursing care.
Johnson's Behavioral System Model
Johnson's Behavioral System Model21)22) is a nursing theory developed by Dorothy E. Johnson 23) in the 1970s. The model focuses on the individual as a system made up of multiple interacting subsystems, such as physiological, psychological, and social subsystems. The model emphasizes the importance of understanding the interactions between these subsystems and the environment in order to promote health and well-being.
The model includes three main components: the individual, the environment, and the nursing process. The individual is seen as a holistic being with unique needs and characteristics. The environment includes the physical, social, and cultural factors that affect the individual's health.
The Behavioral System Model posits that the individual's health and well-being are influenced by the interactions between their various subsystems and the environment. It also posits that the individual has the innate ability to maintain balance and harmony among their subsystems, but that this ability can be affected by environmental stressors.
The model is based on the concept of “goal attainment” which refers to the individual's ability to achieve their goals related to health and well-being. It also posits that the individual's perception of the environment, and their ability to cope with stressors, play a major role in their ability to achieve their goals.
Johnson's Behavioral System Model is widely used in nursing practice, education, and research, and is considered a holistic, person-centered model that promotes health and well-being. It is also considered a useful tool for understanding the complex interactions between the individual, environment, and nursing care.
Parse's Human Becoming Theory
Parse's Human Becoming Theory24)25), also known as the Theory of Human Becoming, is a nursing theory developed by Rosemarie Rizzo Parse in the 1980s. The theory emphasizes the importance of understanding the individual's unique experience of the world and the meaning they attach to it, in order to promote health and well-being.
The model is based on the idea that the individual is a holistic being, made up of physical, psychological, social, and spiritual components. The model posits that health and well-being are maintained through the balance and harmony of these components and that the individual's unique experience of the world and the meaning they attach to it play a major role in this balance.
The model includes four main components: the individual, the environment, health, and nursing. The individual is seen as a holistic being with unique needs and characteristics. The environment includes the physical, social, and cultural factors that affect the individual's health. Health is defined as a state of balance and harmony among the various components of the individual.
The nursing process includes assessment, planning, implementation, and evaluation. The model emphasizes the importance of understanding the individual's unique needs and characteristics and creating a personalized plan of care to promote health and well-being.
The Human Becoming Theory is based on the concept of “human becoming” which refers to the individual's unique experience of the world and the meaning they attach to it. The concept of “human becoming” suggests that individuals are constantly evolving and changing as they interact with their environment. Health is viewed as a process of becoming, rather than a static state, and is defined as the person's ability to engage in the process of becoming. The model emphasizes the importance of the nurse-patient relationship and the nurse's role in facilitating the individual's innate drive toward health and well-being.
Parse's Human Becoming Theory is widely used in nursing practice, education, and research, and is considered a holistic, person-centered model that promotes health and well-being. It is also considered a useful tool for understanding the complex interactions between the individual, environment, and nursing care.
Orlando's Patient-centered Nursing Theory
Orlando's Patient-centered Nursing Theory26)27)28) , also known as the “Deliberative Nursing Process” theory, is a nursing theory developed by Ida Jean Orlando in the 1950s. The theory emphasizes the importance of understanding the individual's unique needs and characteristics and creating a personalized plan of care to promote health and well-being.
The model is based on the idea that the individual is a holistic being, made up of physical, psychological, social, and spiritual components. The model posits that health and well-being are maintained through the balance and harmony of these components, and that the individual's unique needs and characteristics play a major role in this balance.
The nursing process in Orlando's Patient-centered Nursing Theory consists of four steps:
- Identification of patient's needs: This step involves gathering data about the patient's health status, including their physical, psychological, and social well-being. The nurse uses non-directive communication techniques, such as active listening and open-ended questions, to understand the patient's subjective experience of their health and illness.
- Planning: The nurse develops a plan of care that is tailored to the patient's unique needs, values, and beliefs. The plan of care should be flexible and open to change as the patient's needs and goals evolve over time.
- Implementation: The nurse carries out the plan of care, working in partnership with the patient to promote their health and well-being. The nurse also evaluates the effectiveness of the plan of care and makes adjustments as necessary.
- Evaluation: The nurse evaluates the effectiveness of the plan of care in achieving the patient's desired outcomes. The nurse also considers the patient's unique perspective and experiences in making this evaluation.
The nursing process in Orlando's Patient-centered Nursing Theory is an ongoing, iterative process that is focused on understanding the patient as a holistic, dynamic, and constantly changing being. The theory emphasizes the importance of understanding the patient's perspective and experiences, promoting self-care, and working in partnership with the patient to support them in achieving their desired outcomes.
The Orlando's Patient-centered Nursing Theory is widely used in nursing practice, education, and research, and is considered a holistic, person-centered model that promotes health and well-being. It is also considered a useful tool for understanding the complex interactions between the individual, environment, and nursing care.